What is paediatric asthma?
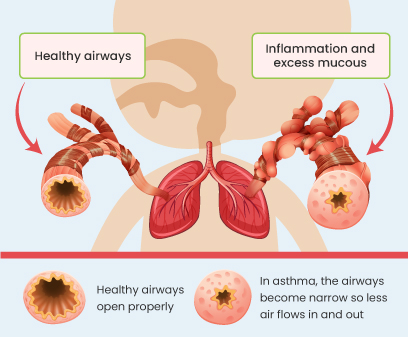
Asthma is a long-term (chronic) condition where your child’s lungs can get irritated by being exposed to various triggers such as cold weather, pollen, etc. When this happens, the inside of the airways swell up, and produce more mucus8 and the muscles around the airways get tight making it difficult for you to breathe.1
Asthma often starts when kids are young,5 and it's more common in boys than girls.6
Fortunately, there are effective treatment options available to manage asthma symptoms and improve their quality of life.
How common is asthma in childhood?
Asthma is a common disease in children. Recent data shows, around 9-10% of children aged 6-14 worldwide have asthma.3
.svg)
.svg)
The burden of asthma in the UAE is 11.9%, being significantly higher in the 6- to 7-year-old group.7
Symptoms of paediatric asthma
.svg)
Recurrent coughing.
.svg)
Have ongoing wheezing (a high-pitched whistling sound made while breathing), especially when sleeping or triggered by activities like crying or laughing.
.svg)
Worsening of asthma symptoms at night or early in the morning.
.svg)
Tightness in their chest or trouble breathing, such as feeling out of breath or breathing quickly.
.svg)
Feeling tired from not sleeping well.
.svg)
Act cranky or easily upset.
These symptoms can vary from being not too bad to very severe. Sometimes, worsening symptoms can lead to severe health risks, indicating a worsening of the condition. During this time, symptoms such as increased wheezing, shortness of breath, coughing (especially at night), lethargy, reduced exercise tolerance may occur. If your child shows any of these signs, it is crucial to seek medical help immediately.4
Triggers of paediatric asthma
.svg)
Viral Infections
Pathogenic agents like viruses can cause infections in the lung passages. Viral infections can cause the airways to become inflamed, leading to wheezing and possibly developing into asthma.8
.svg)
Allergens & Irritants
Your child may have allergies to things like dust and pollen grains. Other factors include dust mites, pet dander, etc., which can trigger their symptoms. Certain environmental triggers, like air pollution, gases, strong odours from coils, cooking smells, sprays, or smoke, can irritate your child's airways and worsen their symptoms.
.svg)
Exercise
Physical activities (strenuous play or exercise) can sometimes cause wheezing, coughing, and a feeling of chest tightness in children with respiratory issues due to the narrowing of airways.
.svg)
Stress & Emotions
When your child feels stressed, it can cause shortness of breath and exacerbate their symptoms.
Risk factors of childhood asthma
Factors that could raise the likelihood of your child developing asthma include:
.svg)
Viral infections can significantly impact both the development and exacerbation of asthma. If your child gets viral infections a lot, it might increase the chances of them developing asthma.8
.svg)
Having previous allergic reactions, i.e., food allergies.
.svg)
A family history of asthma or allergies.
.svg)
Living in areas with a lot of pollution.
.svg)
Being overweight.
.svg)
Having ongoing respiratory issues, such as rhinitis.
.svg)
Maternal obesity and weight gain during pregnancy heighten the likelihood of asthma in offspring.
.svg)
Being around tobacco smoke during pregnancy and childhood raises the risk of developing asthma.
Patients with close family members, like a parent or sibling with asthma or allergies, are more likely to suffer from it.1
Paediatric asthma diagnosis and tests
Diagnosing asthma in children can be tricky, especially when they're young. Asthma symptoms can resemble those of other childhood illnesses, occasionally resulting in inaccurate or mistaken diagnoses.
To diagnose asthma, your child's doctor may use several methods:4,12
.svg)
Physical examination and review of medical history
.svg)
Allergy Tests
(Skin prick or blood tests, especially if there's a history of allergies)
.svg)
Lung function tests
(Spirometry measures how well the lungs are working in children aged ≥5)13
.svg)
Chest X-ray
(To examine the condition of the lungs)
In children <5 years of age, the doctor might recommend a trial of asthma medication for a minimum of 2-3 months to see if the symptoms improve.4, 12
Preventing asthma worsening
To prevent asthma attacks, planning carefully and avoiding things that can trigger them is essential. Here are some tips:
.svg)
Reduce exposure to asthma triggers4,11
Try to keep your child away from things that worsen asthma, such as allergens (house dust mite, furred pets, pest rodents, cockroaches, mold, and pollen) or irritants (car exhaust fumes, smoke, or strong smells).
.svg)
No smoking around your child
Tobacco smoke is a considerable risk for childhood asthma, so keep your child away from it.
.svg)
Treatment as prescribed14
Adherence to doctor-prescribed medications.
.svg)
Encourage physical activity
If your child's asthma is well controlled, regular exercise can improve their lung function. Always consult a doctor to ensure the exercise routine is safe and suitable for your child's condition.
.svg)
Regular check-ups
See your child's doctor regularly. Don't ignore signs that their asthma might not be well controlled.
.svg)
Maintaining a healthy weight
Being overweight can exacerbate asthma and lead to additional health issues. Regular monitoring is essential.4
Paediatric asthma treatment
How doctors handle your child's asthma at the beginning depends on how bad it is.
Treating asthma involves two main steps: stopping symptoms from occurring and dealing with asthma attacks if they do occur.
The type of medicine your child needs depends on their age, what symptoms they have, what triggers their asthma, and what works best to keep them in check.
Asthma medications fall into two categories:
Maintenance medications
These must be taken regularly, regardless of symptoms, to prevent and control symptoms, reduce airway inflammation, and decrease the risk of exacerbations. Inhaled corticosteroids (ICS) are the most commonly prescribed maintenance medications. They reduce chronic inflammation and prevent airway narrowing and shortness of breath. They are taken particularly by inhalation and can be used to treat mild to severe asthma. If asthma isn't well controlled with these, the dose can be increased or combined with other medications. Overall, ICS are safe and should be reviewed on how well it's working as the symptoms of children can change over time to time and need to be checked and adjusted to manage asthma effectively.

Reliever medications
Also known as rescue medications, these are fast-acting medications used as needed to relieve acute symptoms. They provide quick relief during asthma flare-ups and helps in reducing breathing difficulties during exercise. Reducing the need for reliever medications is a key goal in asthma management. Using your reliever more than twice a week indicates poor asthma control. In such cases, long-term controller medications should be taken regularly to address the underlying airway inflammation.13,14,16

Treatment types
.svg)
Inhaled medications can be delivered using different types of devices like dry powder inhalers (DPI), pressurized metered dose inhalers (pMDI). These devices help deliver drugs directly to the lungs.
DPIs contain the drug in a powder form and the child has to inhale deeply and forcefully to get the medicine into the lungs.
pMDIs contain the drug along with a propellant in a liquid or gaseous form and the child has to inhale the medicine slowly and deeply. Add-on devices like spacers or masks may be beneficial for patients who are unable to use their pMDIs correctly.
.svg)
Asthma action plan
.svg)
It helps you recognise severe asthma attacks or worsening symptoms.
.svg)
It helps you understand which medication to administer or how to initiate the treatment.
.svg)
It guides you on when to contact the doctor or seek emergency help by providing telephone, emergency, or hospital contact details
.svg)
Reference:
- World Health Organization. Asthma [Internet]. World Health Organisation. 2023. Available from: Click here
- Plaza-González S, Zabala-Baños M del C, Astasio-Picado Á, Jurado-Palomo J. Psychological and Sociocultural Determinants in Childhood Asthma Disease: Impact on Quality of Life. International Journal of Environmental Research and Public Health [Internet]. 2022 Feb 24;19(5):2652. Available from: Click here
- Singh S, Salvi S, Mangal DK, Singh M, Awasthi S, Mahesh PA, et al. Prevalence, time trends and treatment practices of asthma in India: the Global Asthma Network study. ERJ Open Research [Internet]. 2022 May 30;8(2):00528-2021. Available from:Click here
- Global initiative for Asthma. Global Strategy for Asthma Management and Prevention [Internet]. 2023 Jul. Available from: Click here
- Lizzo JM, Goldin J, Cortes S. Pediatric Asthma. [Updated 2024 May 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Click here
- Gupta S, Daniel R, Aggarwal P, Kalaivani M. Prevalence of asthma among children in India: A systematic review and meta-analysis. Lung India. 2022;39(4):357
- Ibrahim NM, Almarzouqi FI, Al Melaih FA, Farouk H, Alsayed M, AlJassim FM. Prevalence of asthma and allergies among children in the United Arab Emirates: A cross-sectional study. World Allergy Organ J. 2021 Oct 6;14(10):100588.
- Hansbro NG, Horvat JC, Wark PA, Hansbro PM. Understanding the mechanisms of viral induced asthma: New therapeutic directions. Pharmacology & Therapeutics. 2008 Mar;117(3):313–53.
- Salvi SS, Apte KK, Dhar R, Shetty P, Faruqi RA, Thompson PJ, et al. Asthma Insights and Management in India: Lessons Learnt from the Asia Pacific - Asthma Insights and Management (AP-AIM) Study. The Journal of the Association of Physicians of India [Internet]. 2015 Sep 1 [cited 2024 Mar 20];63(9):36–43. Available from: Click here
- Deka H, Mahanta P, Ahmed SJ, Rajbangshi MC, Konwar R, Basumatari B. Risk Factors of Childhood Asthma Among Patients Attending a Tertiary Care Centre in North-East India. Journal of Asthma and Allergy [Internet]. 2022 Sep 14 [cited 2022 Oct 1];15:1293–303. Available from: Click here
- Cheraghi M, Dadgarinejad A, Salvi S. A Cross-Sectional Study to Find Prevalence and Risk Factors for Childhood Asthma in Pune City, India. ISRN Public Health. 2012;2012:1–8.
- Program NAE and P, Asthma TEP on the D and M of. Section 4, Managing Asthma Long Term in Children 0–4 Years of Age and 5–11 Years of Age [Internet]. www.ncbi.nlm.nih.gov. National Heart, Lung, and Blood Institute (US); 2007. Available from: Click here
- Indian Medical Association. Recommendations on Management of Asthma in Primary Care (2020). 2020 Dec 22;1–28.
- Mayo Clinic. Childhood Asthma - Diagnosis and Treatment - Mayo Clinic [Internet]. Mayoclinic.org. 2019. Available from: Click here
- Medication for people with asthma [Internet]. Nih.gov. Institute for Quality and Efficiency in Health Care (IQWiG); 2017. Available from: Click here
- DeVrieze BW, Giwa AO. Peak Flow Rate Measurement [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. Available from: Click here
